August 2, 2025 — eBharat.com News Desk
India’s insurance tech space just got a major upgrade.
Policybazaar for Business (PBFB), the corporate arm of Policybazaar, has launched ClaimSetu — a first-of-its-kind, AI-powered health insurance claims platform built especially for group health insurance (GHI) reimbursements.
This new engine combines artificial intelligence (AI), machine learning, natural language processing (NLP), and OCR (optical character recognition) to simplify what has long been a messy and stressful process for employees and HR teams alike.
What Exactly Is ClaimSetu?
ClaimSetu is designed to handle the entire claims process — from document upload to insurer communication — using AI-based automation. It can read your bills, prescriptions, discharge summaries, and instantly verify if something is missing or incorrect. It doesn’t just track the claim — it also scores it, offering a real-time prediction of how likely it is to be approved based on the policy, documentation, and insurer patterns.
Here’s what makes ClaimSetu different:
| Feature | How It Helps |
|---|---|
| AI-Powered Document Reading | Extracts data from bills, discharge summaries, and medical reports instantly |
| Real-Time Alerts | Flags missing or invalid paperwork on the spot |
| Smart Claims Scoring | Predicts likelihood of approval using AI algorithms |
| Instant Tracking | Live updates via WhatsApp and app notifications |
| HR Dashboard Integration | Gives HR teams full visibility into pending and settled claims |
Why It Matters for Employers and Employees
Let’s be honest — group health insurance claims have always been a headache. You collect physical documents, send them over email, wait for approvals, and deal with unclear rejections.
ClaimSetu cuts through all that chaos.
For HR teams, it reduces back-and-forth, ensures higher claim accuracy, and speeds up resolution. For employees, it offers a clearer, faster, and more transparent experience — something most people have never had when dealing with reimbursement claims.
Policybazaar says ClaimSetu can improve processing speed by up to 50% — that’s a big leap in an industry where delays can often take weeks.
Built With Security & Scalability in Mind
While ClaimSetu currently supports GHI reimbursements, it’s already built to scale to other areas like OPD claims, individual health claims, and more. It also follows enterprise-grade data security protocols, making it safe for large corporates and sensitive health data.
Policybazaar has confirmed that the platform is being rolled out in phases, with early results showing strong improvement in first-time claim success rates.
How Will This Impact You?
Whether you’re an HR professional managing hundreds of claims or an employee trying to get a hospital bill reimbursed — ClaimSetu brings much-needed clarity and speed to the process. It reflects a growing trend of using AI not just for buying insurance, but also managing it better after purchase.
ClaimSetu is not just a tech upgrade — it’s a sign that Indian insurance is finally catching up with the digital-first expectations of today’s workforce. If you’re working in a company with group health coverage, expect your claim experience to feel smoother, faster, and smarter in the months ahead.
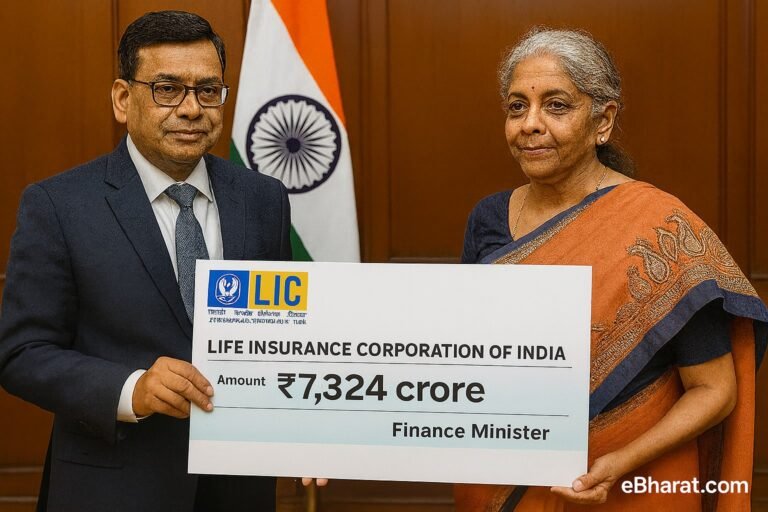
Policybazaar isn’t just launching smart tools like ClaimSetu — it’s also turning that innovation into serious revenue. In fact, the company posted a strong Q1 performance recently. Check out how PolicyBazaar & PaisaBazaar earned ₹85 crore in profit this quarter and what it means for India’s growing fintech space.