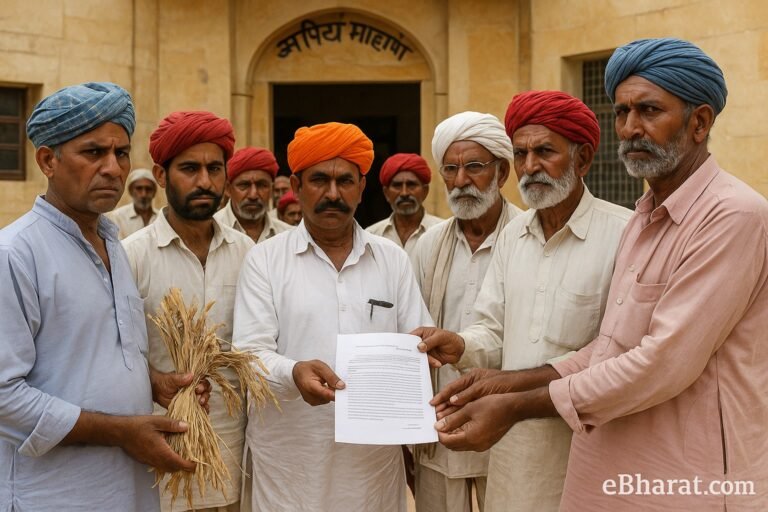
New Delhi, August 29, 2025 — India’s healthcare and insurance sectors are facing a fresh standoff. The Association of Healthcare Providers of India (AHPI) has accused the General Insurance Council (GIC) of using anti-competitive practices to pressure hospitals into lowering treatment tariffs.
At the centre of this conflict is the cashless treatment system, which allows patients to avail hospital services without upfront payment. AHPI claims that insurers are unfairly suspending cashless services for hospitals that refuse to accept reduced tariffs. This has raised alarms for patients who rely heavily on insurance-backed medical care.
What AHPI Is Saying
According to AHPI, hospitals are being pushed into a corner:
- Forced Tariff Cuts: Insurers allegedly demand that hospitals slash their treatment charges below sustainable levels.
- Cashless Service Suspension: Non-compliant hospitals risk losing cashless tie-ups, which directly affects patients.
- Common Empanelment Issue: The council is promoting a one-size-fits-all empanelment system, reducing hospitals’ ability to negotiate terms.
AHPI argues that these practices amount to cartelization, which could eventually hurt both hospitals and patients.
Why It Matters for Patients
For policyholders, the dispute raises real concerns:
- Access to Cashless Care: Patients may be forced to pay upfront if their hospital’s cashless service is suspended.
- Quality of Care: If hospitals accept reduced tariffs, they may cut corners to stay viable.
- Trust Gap: Disputes between insurers and hospitals shake consumer confidence in the healthcare system.
The Legal and Regulatory Angle
Industry experts point out that the Competition Commission of India (CCI) may need to step in if AHPI formally proves cartelization. Additionally, the Insurance Regulatory and Development Authority of India (IRDAI) could be asked to review whether insurers’ practices align with fair-trade principles.
This conflict highlights the tension between controlling healthcare costs and ensuring hospitals remain financially sustainable.
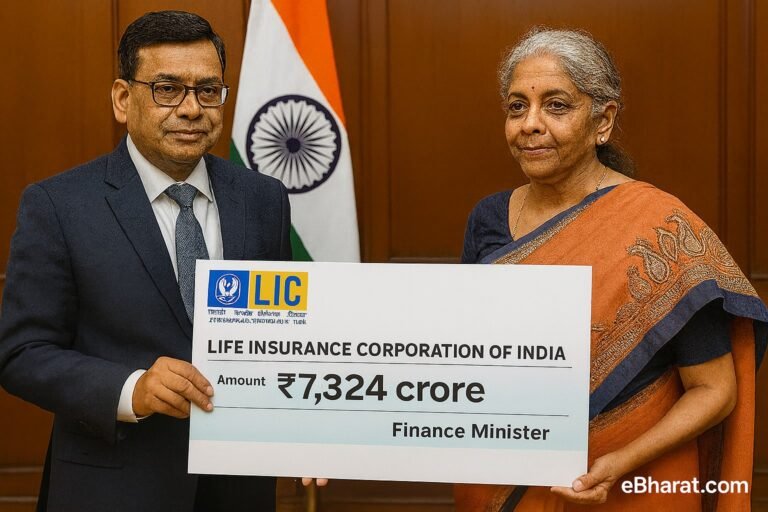
Why It Matters for India’s Insurance Sector
- Patients First: Policymakers must balance cost control with quality care.
- Industry Accountability: Both hospitals and insurers must operate transparently.
- Future of Cashless Care: With nearly 60% of urban policyholders depending on cashless treatment, clarity and fair regulation are urgent needs.
Want to Build a Career in Insurance?
Join our agent network and be part of India’s growing insurance industry. Get training, tools, and full support to succeed.
Apply Now to Become an Agent
Stay tuned with eBharat.com for more updates on healthcare and insurance developments in India.